Directions:
To view this case click on the different case tabs below.
As you tab through the case you will see photos. Click on each photo to see an enlargement.
When you have determined a diagnosis and treatment, select the Discussion tab.
Patient: Adult male.
Chief Complaint:
Patient complains of a sore mouth of eight months duration. The discomfort has consistently involved the labial and buccal mucosa and the tongue. The sores fluctuate in size. The patient states that wearing partial dentures exacerbates the oral discomfort.
Discontinuing colloidal gold medication exacerbated both the oral discomfort and arthritis.
Medical History:
The patient was hospitalized ten months ago for pneumonia, which was successfully treated with antibiotics. Surgeries have included hernia repair, nasal polyp excision, removal of pilonidal cyst, appendectomy, and tonsillectomy. The patient reports rheumatoid arthritis of fifteen years duration, currently treated with Naprosyn. Lichen planus on the skin is treated with a steroid cream. Systemic steroids caused a skin rash, and aspirin causes bleeding problems. The patient reports asthma, alleries to pollen and some foods and medications.
Dental History:
The patient has had partial dentures for eight years, and the current dentures are four years old. The patient hasn't worn the partial dentures for the past six months due to oral discomfort.
Clinical Findings:
The buccal and lingual mucosa is erythematous with areas of epithelial thickening arranged in a lacy line pattern. Focal white plaques which rub off leaving a tender base are present on the mucolabial folds. All lesions are bilateral. Scaly white plaques on an erythematous base are present bilaterally on the palms, wrists, and elbows. Some of the white plaques have a lacy line pattern. The white epithelial thickening lesions on the skin and buccal and labial mucosa are thickened, firm, and rough to palpation. They do not rub off and are fixed to the surface mucosa. Ulcers on the lower lip are covered by firm crusts. Ulcers on the lower lip and buccal and lingual mucosa are tender to palpation.
| Clinical Images | |
|---|---|
 |
 |
| Palm and Wrist | Close-up of Lesions on Palm |
 |
 |
| Lesions on the Elbow | Lips |
 |
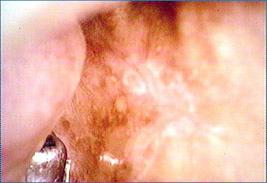 |
| Left Buccal Mucosa | Left Buccal Mucosa |
 |
|
| Left Lateral and Ventral Tongue | |
There are no radiographs available for this case.
There are no lab reports available for this case.
There are no charts available for this case.
Summary:
The patient has vesicular-ulcerated-erythematous lesions consisting of:
~Persistent multiple painful ulcers
~Tender erythematous mucosa
~White surface lesions.
The patient also has ulcers and crusts of the skin.
Lesions to Exclude from the Differential Diagnosis:
Hereditary
~Epidermolysis Bullosa
*Begin at birth or early childhood.
Viral infections
~Have acute onset and resolution with cervical lymphadenopathy.
Idiopathic Diseases
~Aphthous Ulcers
*Lesions have acute or abrupt onset and heal.
~Erythema Multiforme
*Acute onset with healing
~Epithelial Dysplasia, Carcinoma-in-situ, and squamous cell carcinoma
*Typically not as persistently painful
~Contact stomatitis
*No history of contact with cinnamon, dentifrices, mouthrinses or other agents that commonly cause this.
Lesions to Include in the Differential Diagnosis:
Candidosis
~White plaques which rub off leaving a tender base
Lichen Planus
~Lacy line pattern of white epithlelial thickening
~Multiple ulcers are often present in lichen planus.
~Skin lesions typical of lichen planus are present
Lupus Erythematosus
~Can have painful oral mucosal ulcers
~Lupus erythematous may have skin lesions similar to this patient.
Management:
Since Candidosis is in the differential diagnosis, attempt to treat this first with antifungal agents to help arrive at a definitive diagnosis.
The antifungal medications resolved some of the lesions. An incisional biopsy of the white thickened lesions was performed and diagnosed as lichen planus.
The patient was educated about the nature of lichen planus emphasizing that the disease can be controlled with steroid medication but not cured. A topical steroid mouthrinse should be attempted initially. Candidosis is a common complication of lichen planus and needs to be treated with antifungal medication when it occurs.
Final Diagnosis:
Lichen planus of oral mucosa and skin and candidosis